 We have all heard the phrase and it usually is a reference to someone who is just a little less on top of their game. Just last week, however, The New York Times released data on staffing in nursing homes that showed a tremendous variance in staffing levels on their units based on time of day and time of week.
We have all heard the phrase and it usually is a reference to someone who is just a little less on top of their game. Just last week, however, The New York Times released data on staffing in nursing homes that showed a tremendous variance in staffing levels on their units based on time of day and time of week.
These staff levels are not inconsequential, because when we talk generically about “nursing homes,” we may be making reference to assisted living or skilled nursing or other supportive living facilities. This is all a way to say that the residents need help with any number of their key activities of daily living like toileting, dressing, bathing, eating and walking, etc. The New York Times reported variances from fully staffed to the understaffed weekends to be as much as a 100 percent difference. That is to say that the number of nurses or aides covering the residents on weekends was as little as half the number as during weekdays.
Before the Affordable Care Act, nursing homes self-reported their staffing levels to the government watchdog agencies. Whatever they said was what was on record, so less ethical organizations could easily game a system where no one was minding the store. Since the ACA in 2010, these numbers are now verified. While ACA now more closely monitors staffing, there can still be day to day variances that may elude detection. Some defenders of the status quo claim that on weekends more family are visiting their loved ones allowing thinner staff to keep up with what is alleged to be lower demand. Maybe? How many visiting sons are comfortable helping mom to the toilet?
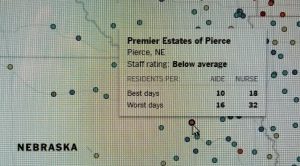
If your older loved one is one of the 1.4 million Americans who are a resident in a nursing home, you can check on their staffing variances. The New York Times actually published a map on line that allows you to hold your cursor over a specific facility on the map to see how they rate from “much above average” to as low as “much below average.” They also will note for you the low and high resident to staff ratios of both nurses and aides. I have in our inset a picture of a facility in Nebraska as an example.
So, do three things if you are helping a loved one move to, or have one already in, a nursing home…or may have one moving anytime soon:
- Go to the map to get the data and also those of competing facilities around the region where your loved one may move;
- Get references on facilities from care managers or other health care professionals from your locale; and
- Once your loved one moves in, drop by as frequently as you can, but do so at different times of the day or week.
Consider all of these as steps toward catching a facility in the act of doing things right. If not, don’t be afraid to make a change of venue and a change for the better for you and your loved one.
Charlotte Bishop is an Aging Life Care Advisor, Geriatric Care Manager and founder of Creative Care Management, certified professionals who are geriatric advocates, resources, counselors and friends to older adults and their families in metropolitan Chicago. She also is the co-author of How Do I Know You? A Caregiver’s Lifesaver for Dealing with Dementia.





